Share this article on social media
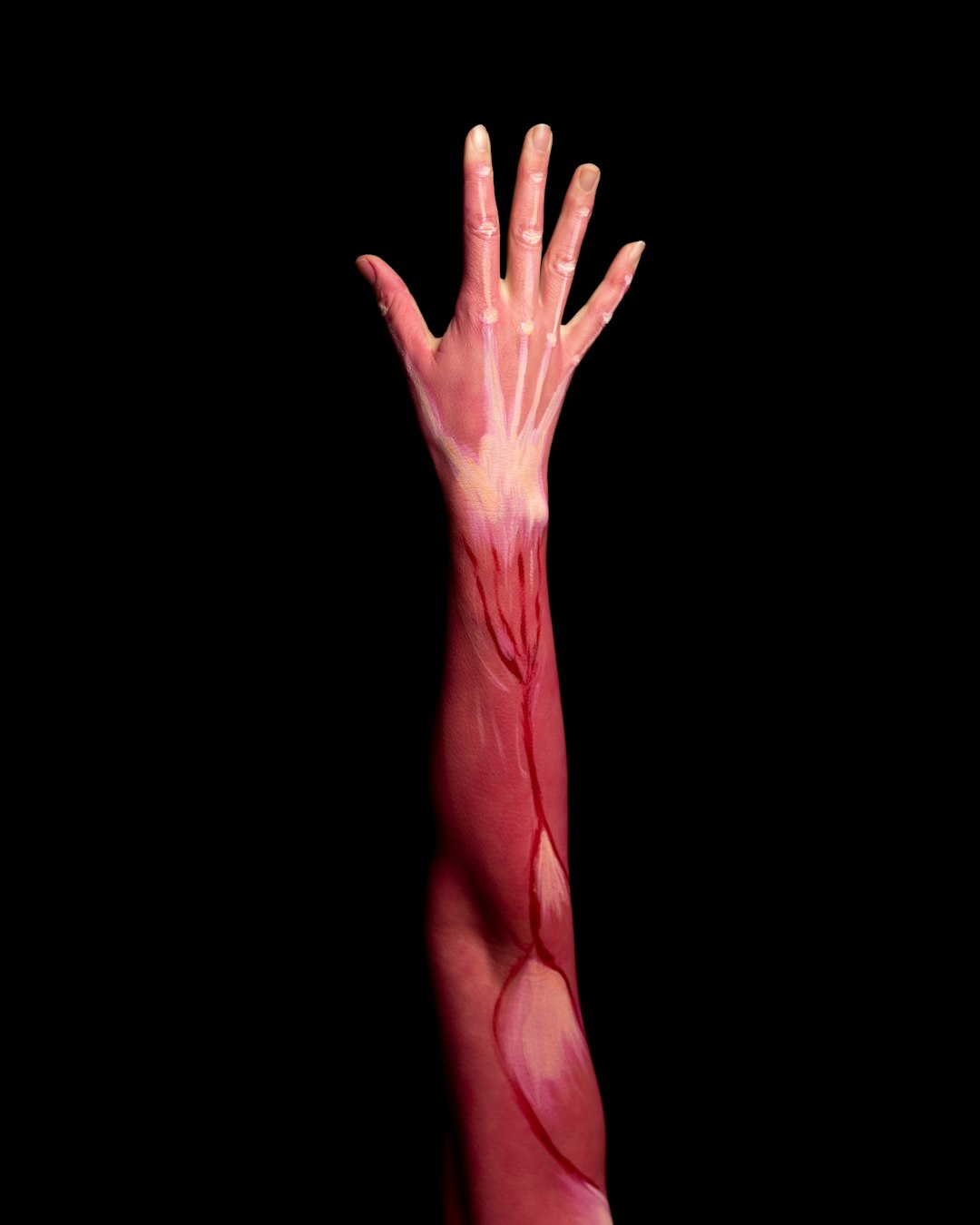
Confronting the harsh reality of different types of muscle diseases can be overwhelming for individuals and families. Understanding the intricacies of these conditions, such as muscular dystrophy, myasthenia gravis, amyotrophic lateral sclerosis (ALS), and polymyositis, is crucial for early detection and effective management. Recognizing the signs and symptoms, exploring diagnosis and treatment options, as well as finding support and resources can make a significant difference in coping and living with these challenges.
Understanding Muscle Diseases
Muscle diseases, also known as myopathies, encompass a range of conditions that affect the muscular system. These diseases can manifest in various forms, impacting muscle function and overall mobility. Understanding the complexities of these conditions is crucial in providing effective care and support to individuals affected by them.
What Are Muscle Diseases?
Muscle diseases refer to a group of disorders that affect the skeletal muscles, smooth muscles, or cardiac muscles. These conditions can be categorized based on their causes, such as genetic, autoimmune, inflammatory, or neurological factors.
Types of Muscle Diseases
- Genetic Muscle Diseases: These are inherited conditions, such as muscular dystrophy, that result from mutations in genes responsible for muscle structure and function.
- Autoimmune Muscle Diseases: Conditions like myasthenia gravis involve the immune system mistakenly attacking the body’s own muscles, leading to muscle weakness and fatigue.
- Neurological Muscle Diseases: Amyotrophic lateral sclerosis (ALS) is an example of a neurological disorder that affects nerve cells controlling voluntary muscles, leading to muscle degeneration.
- Inflammatory Muscle Diseases: Polymyositis is an inflammatory myopathy characterized by muscle weakness and inflammation.
Impact on Individuals
Muscle diseases can have a significant impact on an individual’s quality of life, often causing challenges related to mobility, coordination, and strength. The specific symptoms and severity can vary depending on the type of muscle disease and individual factors.
Understanding the distinct characteristics of each type of muscle disease is crucial for accurate diagnosis and effective management. It enables healthcare professionals to tailor treatment plans and support strategies that address the unique needs of individuals living with these conditions.
Types of Muscle Diseases
When it comes to types of muscle diseases, it’s essential to understand the various conditions that can affect the muscular system. Here are some of the most common types:
Muscular Dystrophy:
- This genetic disease leads to the progressive weakening and degeneration of the body’s muscles over time.
- It primarily affects voluntary muscles, causing difficulties in mobility and coordination.
- There are several types of muscular dystrophy, each with its own specific symptoms and severity.
Myasthenia Gravis:
- This autoimmune disorder disrupts the communication between nerves and muscles.
- It results in muscle weakness and fatigue, particularly in the facial muscles, making activities like chewing and swallowing challenging.
- Symptoms may vary in severity and can worsen with physical activity.
Amyotrophic Lateral Sclerosis (ALS):
- Also known as Lou Gehrig’s disease, ALS affects nerve cells that control voluntary muscle movement.
- It leads to muscle weakness, paralysis, and eventually respiratory failure.
- ALS progresses rapidly, making daily tasks increasingly difficult for individuals affected by the condition.
Polymyositis:
- This inflammatory muscle disease causes weakness and inflammation in the muscles.
- It especially affects the hips, thighs, shoulders, and upper arms.
- Individuals with polymyositis may experience difficulties in climbing stairs, lifting objects, and getting up from a seated position.
Comparing these types of muscle diseases reveals the unique ways in which they impact the muscular system, highlighting the importance of accurate diagnosis and targeted treatment approaches. Each condition requires a tailored management plan to address its specific symptoms and progression.
Muscular Dystrophy
Muscular Dystrophy is a group of genetic diseases characterized by progressive weakness and degeneration of the body’s muscles. It is one of the most well-known types of muscle diseases and can manifest in different forms, each with its own specific symptoms and patterns of inheritance. Here’s a closer look at the different types of muscular dystrophy:
Duchenne Muscular Dystrophy (DMD)
- Occurs predominantly in males
- Typically diagnosed in early childhood
- Rapid progression of muscle weakness
- Wheelchair dependency often occurs by the teenage years
Becker Muscular Dystrophy (BMD)
- Similar symptoms to DMD but with a later onset and slower progression
- Some individuals retain the ability to walk into their 30s or beyond
Facioscapulohumeral Muscular Dystrophy (FSHD)
- Weakness begins in the face, shoulder blades, and upper arms
- Symptoms may appear in adolescence or early adulthood
- Disease progression varies widely, even among family members
Myotonic Dystrophy
- Characterized by prolonged muscle contractions, cataracts, heart conduction defects, and endocrine changes
- Two types: DM1 and DM2, each caused by a different genetic mutation
Comparison Table:
| Type of Muscular Dystrophy | Onset | Progression | Genetic Inheritance |
|---|---|---|---|
| Duchenne (DMD) | Early childhood | Rapid | X-linked recessive |
| Becker (BMD) | Later onset | Slower | X-linked recessive |
| Facioscapulohumeral (FSHD) | Adolescence/adulthood | Variable | Autosomal dominant |
| Myotonic (DM1/DM2) | Variable, usually adulthood | Variable | Autosomal dominant |
Understanding the specific features and differences among these types of muscular dystrophy is crucial in providing appropriate care and support for affected individuals and their families. Early diagnosis and intervention play a significant role in managing the symptoms and improving the quality of life for those with muscular dystrophy.
Myasthenia Gravis
Myasthenia Gravis is a chronic autoimmune neuromuscular disease that leads to varying degrees of skeletal muscle weakness. This condition is caused by a communication breakdown between nerves and muscles, resulting in muscle fatigue and weakness. Here’s a detailed look at Myasthenia Gravis and how it differs from other types of muscle diseases:
Characteristics of Myasthenia Gravis:
- Gradual weakness of the muscles, especially those that control eye and eyelid movement, facial expression, chewing, talking, and swallowing.
- Muscle weakness worsens with activity and improves with rest.
- Symptoms can fluctuate, with periods of exacerbation and remission.
Comparison with Other Muscle Diseases:
| Aspect | Myasthenia Gravis | Other Muscle Diseases |
|---|---|---|
| Cause | Autoimmune disorder affecting the neuromuscular junction | Various causes including genetic, inflammatory, and metabolic factors |
| Specific Muscle Affected | Typically affects muscles controlling eye, face, and throat movements | Variable muscle groups affected depending on the specific disease |
| Pattern of Weakness | Fatigability of muscles with use | Progressive weakness over time |
| Response to Treatment | Often shows improvement with acetylcholinesterase inhibitors and immunosuppressive drugs | Treatment varies based on the specific type of muscle disease |
Key Points about Myasthenia Gravis:
- It is not directly inherited nor is it contagious.
- Individuals with Myasthenia Gravis can lead fulfilling lives with proper treatment and management.
- Early diagnosis and management are crucial in improving quality of life and minimizing complications.
By understanding the distinct characteristics of Myasthenia Gravis compared to other muscle diseases, individuals and their families can better comprehend the condition and its management.
In the context of “types of muscle diseases”, awareness of Myasthenia Gravis serves as an essential aspect in recognizing and addressing the diverse challenges posed by muscle-related disorders.
Amyotrophic Lateral Sclerosis (ALS)
Amyotrophic Lateral Sclerosis (ALS), also known as Lou Gehrig’s disease, is a progressive neurodegenerative disorder that affects the nerve cells in the brain and spinal cord, leading to the degeneration of motor neurons. Here are some key points to understand about ALS:
Characteristics: ALS primarily impacts voluntary muscle movement, eventually causing muscle weakness and atrophy. It can affect various aspects of daily life, including walking, speaking, swallowing, and eventually breathing.
Progression: The progression of ALS varies from person to person, but it generally leads to increasing disability over time. Individuals with ALS may experience a loss of independence as the disease advances.
Causes: The exact causes of ALS are not fully understood, although both genetic and environmental factors may play a role. Research suggests that a combination of genetic predisposition and external triggers may contribute to the development of ALS.
Management: Currently, there is no cure for ALS, but various treatments and therapies aim to manage symptoms, maintain function, and improve quality of life. This may include medication, physical therapy, speech therapy, and assistive devices.
Support: Individuals with ALS, along with their families and caregivers, often require significant support to cope with the physical, emotional, and financial challenges associated with the disease. Access to support groups, counseling, and specialized care services can make a meaningful difference in their journey.
In comparison to other muscle diseases, ALS stands out due to its specific impact on motor neurons and the unique challenges it presents in terms of management and support. Understanding the distinct characteristics of ALS is crucial for both patients and caregivers in navigating the complexities of this particular type of muscle disease.
Polymyositis
Polymyositis is a rare type of autoimmune muscle disease that causes inflammation and weakness in the muscles. This condition primarily affects the skeletal muscles, leading to difficulties in performing everyday activities. Here are some key points to understand about polymyositis:
Symptoms: Individuals with polymyositis may experience muscle weakness, particularly in the hips, thighs, shoulders, and upper arms. They may also have difficulty rising from a seated position, climbing stairs, lifting objects, and performing other tasks that involve muscle strength.
Causes: The exact cause of polymyositis is not fully understood, but it is believed to involve an abnormal immune response targeting the body’s own muscles. Environmental factors and genetic predisposition may also play a role in the development of this condition.
Diagnosis: Diagnosis of polymyositis typically involves a combination of medical history review, physical examination, blood tests to check for elevated muscle enzymes, electromyography (EMG) to assess electrical activity in muscles, and muscle biopsy to examine muscle tissue for signs of inflammation.
Treatment: Management of polymyositis often involves a combination of corticosteroids and immunosuppressant medications to reduce inflammation and suppress the immune system’s response. Physical therapy and regular exercise are also essential to maintain muscle strength and function.
Prognosis: With early diagnosis and appropriate treatment, many individuals with polymyositis can experience significant improvement in muscle strength and function. However, long-term management and monitoring are often necessary to prevent disease flare-ups and complications.
In comparison to other types of muscle diseases, polymyositis presents its own unique set of challenges and considerations. Understanding the specific characteristics of polymyositis is crucial in providing comprehensive support and care for individuals living with this condition.
Signs and Symptoms of Muscle Diseases
Muscle diseases encompass a range of conditions, each with its own set of signs and symptoms. Recognizing the specific indicators for different types of muscle diseases is crucial for timely diagnosis and intervention. Here are some common signs and symptoms associated with various muscle diseases:
Muscular Dystrophy:
- Progressive muscle weakness
- Poor muscle tone
- Delayed motor skill development in children
Myasthenia Gravis:
- Muscle weakness that worsens with activity and improves with rest
- Drooping of the eyelids
- Difficulty in swallowing and speaking
Amyotrophic Lateral Sclerosis (ALS):
- Muscle cramps and twitching
- Progressive muscle weakness
- Difficulty in breathing and swallowing
Polymyositis:
- Muscle weakness in the hips, thighs, shoulders, and upper arms
- Difficulty rising from a seated position
- Unintentional weight loss
It’s important to note that the signs and symptoms may vary in intensity and manifestation from person to person, depending on the specific type of muscle disease. Additionally, some muscle diseases may also present with non-muscular symptoms such as cardiac or respiratory issues. If you or a loved one experience any of these signs and symptoms, seeking medical evaluation and intervention is crucial.
Understanding the distinct symptoms associated with each type of muscle disease is essential for early detection and management. These signs serve as critical indicators and can prompt individuals to seek medical attention, leading to timely diagnosis and appropriate treatment plans.
Diagnosis and Treatment Options
When it comes to addressing types of muscle diseases, accurate diagnosis and tailored treatment plans are crucial for managing the conditions effectively. The process involves a combination of medical assessments, specialized tests, and collaborative efforts between healthcare professionals and patients. Let’s delve into the diagnosis and treatment options for the various types of muscle diseases:
Muscular Dystrophy
- Diagnosis: Genetic testing, muscle biopsy, creatine kinase (CK) levels
- Treatment: Physical therapy, orthopedic interventions, respiratory support, medications for symptom management
Myasthenia Gravis
- Diagnosis: Physical exam, blood tests for acetylcholine receptor antibodies, electromyography (EMG)
- Treatment: Cholinesterase inhibitors, immunosuppressive drugs, thymectomy, supportive therapies
Amyotrophic Lateral Sclerosis (ALS)
- Diagnosis: Clinical assessments, electromyography (EMG), nerve conduction studies, MRI
- Treatment: Riluzole, edaravone, physical therapy, speech therapy, breathing support
Polymyositis
- Diagnosis: Muscle biopsy, blood tests for muscle enzymes, electromyography (EMG)
- Treatment: Corticosteroids, immunosuppressive drugs, physical therapy, assistive devices
In the case of muscle diseases, early diagnosis offers the best prospects for managing symptoms and slowing progression. Treatment plans often encompass a multidisciplinary approach, involving neurologists, physical therapists, occupational therapists, and other specialists. Moreover, ongoing research and clinical trials continue to explore novel therapeutic avenues, offering hope for improved outcomes in the future.
Coping and Living with Muscle Diseases
Living with muscle diseases can be challenging, but there are strategies and support systems that can help individuals cope and improve their quality of life. Here are some ways to cope and live with types of muscle diseases:
Physical Therapy and Exercise: Engaging in physical therapy and regular exercise can help maintain muscle strength and flexibility, and improve overall function. This can include low-impact exercises, stretching, and range-of-motion activities tailored to individual needs.
Assistive Devices: Utilizing assistive devices such as braces, canes, walkers, and wheelchairs can provide support and enhance mobility, making daily activities more manageable.
Adaptive Living: Making modifications to living spaces, such as installing handrails, ramps, and lifts, can improve accessibility and safety within the home environment.
Emotional Support: Seeking counseling or joining support groups can offer emotional support and a sense of community. It provides individuals and families with the opportunity to connect, share experiences, and gain valuable insights from others in similar situations.
Nutritional Support: Maintaining a balanced diet with the help of a nutritionist can support overall health and energy levels. For some muscle diseases, specific dietary modifications may be necessary to address unique nutritional needs.
Pacing Activities: Managing and pacing daily activities is important to avoid overexertion and fatigue, which can exacerbate symptoms.
Pain Management: Exploring various pain management techniques, including medication, physical therapy, and alternative therapies, can help alleviate discomfort associated with muscle diseases.
It’s important for individuals with types of muscle diseases to work closely with their healthcare team to develop a tailored approach to coping and living with the condition. Additionally, tapping into available resources and building a strong support network can significantly enhance the overall well-being of those affected.
Support and Resources for Individuals and Families
Dealing with the impact of muscle diseases can be overwhelming for both individuals and their families. Fortunately, there are numerous support systems and resources available to help navigate the challenges that come with these conditions. Here are some valuable support options and resources to consider:
Support Groups: Connecting with others who are facing similar challenges can provide a sense of community and understanding. Many organizations offer support groups specifically tailored to different types of muscle diseases. These groups can offer emotional support, practical advice, and a platform to share experiences.
Educational Workshops: Participating in educational workshops can empower individuals and families by providing valuable information about specific muscle diseases, treatment options, and coping strategies. These workshops are often organized by medical centers and advocacy groups.
Online Forums and Social Media: Engaging in online forums and social media groups dedicated to muscle diseases can offer a virtual support network. These platforms can be a source of ongoing encouragement, information exchange, and a way to stay updated on the latest research and developments.
Counseling and Mental Health Services: It is essential to address the emotional impact of muscle diseases. Seeking counseling or mental health services can provide valuable support for emotional well-being and coping with the challenges of living with a muscle disease.
Financial and Practical Assistance: Many organizations offer financial assistance, ensure access to necessary medical equipment and resources, and provide guidance on navigating insurance and disability benefits.
Caregiver Support: Caregivers play a crucial role in supporting individuals with muscle diseases. Providing resources and support for caregivers, including respite care options and caregiver support groups, is vital in ensuring the well-being of both the patient and their caregivers.
Accessing these support and resources can make a significant difference in the lives of individuals and families affected by muscle diseases, providing essential assistance and understanding in navigating the complexities of these conditions.
Frequently Asked Questions
What are the different types of muscle diseases?
There are various types of muscle diseases, including muscular dystrophy, myasthenia gravis, dermatomyositis, amyotrophic lateral sclerosis (ALS), and polymyositis, among others. Each type has its own set of symptoms, causes, and treatments.
What are the common symptoms of muscle diseases?
Common symptoms of muscle diseases include muscle weakness, muscle degeneration, fatigue, difficulty swallowing, muscle pain, and involuntary muscle contractions. However, the specific symptoms can vary depending on the type of muscle disease.
How are muscle diseases diagnosed?
The diagnosis of muscle diseases often involves a combination of physical examination, medical history review, blood tests, genetic testing, electromyography (EMG), muscle biopsy, and imaging tests such as MRI. These diagnostic tools help to determine the type and severity of the muscle disease.
Are muscle diseases treatable?
While there is no cure for most muscle diseases, treatments such as physical therapy, medication, occupational therapy, assistive devices, and respiratory therapy can help manage symptoms, improve quality of life, and slow the progression of the disease.
Can muscle diseases be prevented?
Many muscle diseases are genetic or have unknown causes, so prevention may not always be possible. However, maintaining a healthy lifestyle, avoiding known risk factors, and seeking early medical attention for symptoms can help reduce the risk of muscle diseases and their complications.